Which fuels are driving cancer cell growth?
And can these fuels be targeted as a therapeutic approach?
If you’re a frequent watcher of Dr. Thomas Seyfried’s podcasts or YouTube videos, you know that before diving into anything related to cancer—whether research or treatment—it’s crucial to start with a clear definition of what cancer is. Simply put, cancer is a disease of uncontrolled cell division. These rapidly proliferating cells can become highly invasive, forming tumors and metastases that ultimately can lead to organ failure and death. While there’s general consensus in the cancer research community about what cancer is, defining how it arises remains far more contested.
The dominant theory in the field, known as the somatic mutation theory (SMT), proposes that cancer develops through the accumulation of genetic mutations—a view shaped by the frequent observation of heavily mutated nuclei in cancer cells. The SMT posits that the uncontrolled cell division characteristic of cancer is driven by a faulty genome, in which mutations disrupt key regulatory genes that normally govern cell growth, repair, and death. Accordingly, research and treatment have largely focused on identifying and targeting these mutations—whether inherited or acquired through age or environmental exposure.
But after decades of working within this framework, serious limitations have become apparent. For example, tumors are often genetically chaotic, yet similar in behavior; some cancers lack clear “driver” mutations, while some healthy tissues contain them. Moreover, growth becomes regulated when the nucleus of a cancer cell is placed into the cytoplasm of a normal cell containing healthy mitochondria. These findings, when viewed together, indicate that nuclear mutations are not the drivers of dysregulated cancer cell growth. Despite enormous investment in mutation-targeted therapies, mortality remains high. In fact, our most meaningful reduction in cancer deaths has come not from treatment but from prevention, like anti-smoking efforts.
Chasing mutations as a strategy to manage cancer is, and will likely remain, a never-ending pursuit—a wild goose chase that eludes capture, though not without great profit along the way.
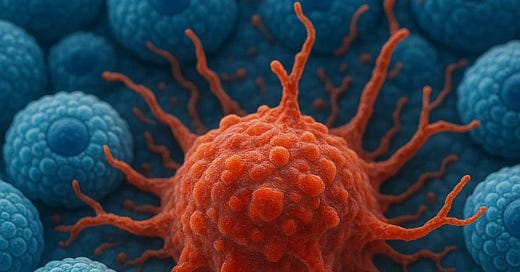
The alternative framework, the mitochondrial metabolic theory (MMT), addresses the observational gaps left by the somatic mutation theory by shifting focus to what may be cancer’s true foundation: dysfunctional energy metabolism as the driver of uncontrolled cell division. The MMT proposes that cancer is fundamentally a metabolic disease, driven by chronically impaired mitochondrial respiration. As a result, cancer cells rely primarily on fermentation of glucose and glutamine to meet their energy demands—even in the presence of oxygen. Unlike the genetic chaos that varies from tumor to tumor (and cell to cell), this metabolic dependency is a consistent feature shared across all major cancer types (and cells).
We ask you now, the reader, should we direct our efforts toward the countless features that make each cancer distinct, or toward the common thread that unites them all?
At the Seyfried Lab, we believe the answer is clear. The path to effective cancer management is to target the energy metabolism of the tumor while maintaining the health and vitality of the patient. Standard clinical therapies can be used only if necessary and modified to reduce toxicity. This is why, over decades of research, we have interrogated cancer cells in vitro to ascertain which fuels are both necessary and sufficient for growth. Taking in the earliest observations from pioneer scientist Otto Warburg—who first discovered that cancer cells ferment the sugar glucose even in the presence of oxygen—we have expanded the metabolic lens in showing that cancer cells not only ferment glucose but also ferment the amino acid glutamine, making glucose and glutamine the twin pillars of tumor bioenergetics.
Our work builds on this foundation by asking not only what cancer cells consume, but what they require. What happens when glucose is removed? When glutamine is withheld? When oxygen is restricted? What remains when a cancer cell is stripped to its barest metabolic needs? These are the questions that drive our research—and, we believe, hold the key to understanding how cancer survives, adapts, and ultimately, how it can be managed.
Derek Lee, a fifth-year PhD candidate in the lab, led a recent study titled Amino Acid and Glucose Fermentation Maintain ATP Content in Mouse and Human Malignant Glioma Cells, which explored these very questions. In this study, we tested multiple glioma cell lines across species to see how they sustain ATP production when deprived of glucose, glutamine, or oxygen. What we found was striking: glucose and glutamine were the most important sugar and amino acid, respectively, for maintaining viability, and notably, glutamine could maintain sufficient ATP levels even under severe hypoxia and in the absence of glucose, where oxidative phosphorylation and glycolysis are essentially offline. Importantly, other amino acids were unable to replace glutamine in producing ATP energy for the cancer cells.
The findings support a central claim of the mitochondrial metabolic theory: that cancer cells survive and proliferate not necessarily because of mutations, but because of their ability to produce energy with little or no oxygen. In other words cancer cells predominantly use fermentation rather than OxPhos for ATP production. And not just glucose—as traditionally emphasized—but also glutamine, a fact too often overlooked. Derek’s work underscores the dependency on fermentation metabolism as the defining feature of cancer metabolism and provides a clear experimental framework for identifying which fuels sustain malignancy, and which interventions may begin to target this vulnerability. To further unpack the implications of the study, Derek Lee will provide insight on his paper and answer the three questions below:
For people who may not be familiar with cancer metabolism, can you explain why it was so important that glioma cells could still survive/remain viable on glutamine alone—even without oxygen?
Derek Lee: Most of the field accepts that glutamine is a very important fuel for all cancer cells. Every culture medium requires it – a fact known since the early work of Eagle in the mid-1900s. However, many will say that glutamine is used exclusively as a fuel for oxidative phosphorylation. My study tried to examine this assumption.
The mitochondria produce ATP in two ways. First, the TCA cycle produces reducing equivalents (NADH and succinate) which are utilized by the electron transport chain complexes to generate energy through oxidative phosphorylation (OxPhos). However, all major cancers have documented abnormalities in the number, structure, or function of mitochondria. OxPhos is a highly coordinated process that relies on the structure of the mitochondria. It stands to reason if the structure is damaged, OxPhos functionality is also compromised.
The second method is through mitochondrial substrate level phosphorylation (mSLP). mSLP occurs during the conversion of succinyl-CoA to succinate. This reaction produces ATP in an oxygen- and structure-independent manner. Given that many cancer cells are in hypoxic environments and have structural abnormalities, it stands to reason that mSLP may be responsible for a significant portion of the ATP content in cancer cell mitochondria.
Indeed, this is what my experiments found. In glioma cells devoid of oxygen and glucose, cells still maintained sufficient ATP to stay viable. This suggests that mSLP must be taken into consideration when examining mitochondrial bioenergetics in cancer cells.
Your study highlights the central role of glutamine in sustaining ATP production, even under hypoxic conditions and in the absence of glucose. What do you think this reveals about the true metabolic priorities of glioma cells?
DL: Cancer is defined as cell division out of control. Cancer cells require both energy (ATP) and biomass (proteins, nucleotides, carbon, etc.) in order to proliferate at a high rate. Glucose supplies both energy through cytosolic substrate level phosphorylation and carbon for biomass synthesis, whereas glutamine supplies both energy through mitochondrial substrate level phosphorylation and carbon plus nitrogen for biomass. The intricate synergy between these two pathways, i.e. glycolysis and glutaminolysis, is what facilitates the cancer phenotype.
How could this research help shape future treatments for brain cancer patients, and of all cancer patients? Are we looking at something that could work alongside existing therapies, or even change the way we think about treatment altogether?
DL: My study emphasizes the distinct bioenergetic difference between the mitochondria in a cancer cells versus a normal cell. Cancer cells produce the majority of their ATP using fermentation, or substrate level phosphorylation. Conversely, normal cells produce the majority of their ATP using oxidative phosphorylation. This tells us that we can use metabolic approaches to target cancer cells in a more specific manner.
For example, we can use calorie-restricted ketogenic diets to lower the amount of glucose in the body. There is no biological requirement for exogenous carbohydrates. Gluconeogenesis will supply enough glucose for normal function and cells which cannot use other fuels (such as erythrocytes). When blood glucose remains low, the body will liberate free fatty acids from adipose tissue and convert them to ketone bodies in the liver. Ketone bodies are an efficient fuel source for cells that use oxidative phosphorylation (such as healthy, quiescent cells). On the other hand, glutamine cannot be targeted with dietary approaches. Pharmacological agents are needed to suppress glutamine concentration or utilization. These agents are being worked on both in our lab and others.
I want to emphasize that while we have significant concerns about some of the standards of care in oncology, our approach is not mutually exclusive to the conventional approach. We have seen unbelievable results in both case reports and clinical trials of individuals who utilized nutritional ketosis alongside the standard of care for a given cancer type. I believe there is incredible value in allowing a patient to become an active participant in their treatment journey.
So, what is the bottom line? Critics of targeting cancer’s metabolic vulnerabilities through fasting or ketogenic diets often argue that glucose is the body’s preferred fuel and that you can’t lower blood sugar to zero. However, as Derek mentioned, carbohydrates are not on the list of essential nutrients while gluconeogenesis can provide the minimal levels needed for the function of red blood cells, which lack mitochondria. Consequently, we can put cancer cells in direct competition with healthy cells for glucose—by lowering blood sugar and elevating blood ketones. In fact, for those exercising frequently and strenuously, glucose and glutamine in the bloodstream will be taken up by muscles and the brain, furthering the competition with the tumor.
Targeting the two essential fuels of glucose and glutamine is an avenue that will necessarily involve all aspects of care—from nutrition to lifestyle and exercise changes to pharmacological intervention—pushing cancer care closer to a model of restorative health, rather than the prevailing paradigm of controlled harm. We cannot wait to continue pushing this research forward and making it accessible to all who need it - for that reason, we want YOUR feedback!
As we plan to increase our activity on Substack, which content would you most benefit from/enjoy?


Thanks for sharing. As a medical oncologist I am very interested in research on optimizing metabolic health and reduction in risk of cancer.
In my practice, we have started a prevention clinic that discusses different approaches to diet and exercise to reduce the risk of cancer.
I’m also interested in the therapeutic potential of ketosis in combination with standard therapies or targeted therapies such as PIK3CA inhibitors, etc.
Feel free to reach out to me on Substack, happy to collaborate and share ideas.
Layperson here but I thought glutamine was always a positive in metabolic health. This sounds like cancer cells love it like they love glucose. Confused.